SATURDAY, 11 OCTOBER 2014
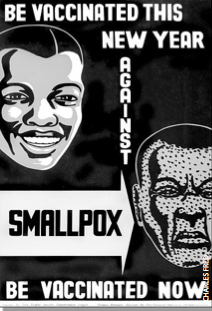
The only infectious disease to have been eradicated world-wide is smallpox. It took an enormous international effort and a highly effective vaccine. Virus eradication is always the ultimate goal for any vaccination program, as it is the only way to ensure a virus doesn’t re- emerge. Measles is a respiratory infection caused by the morbillivirus, and like many viruses it is spread by coughing and sneezing, and is highly contagious. Infection causes a very high fever and a distinctive spot-rash that covers the whole body. Complications during infection can occur in many children; one in 10 get an ear infection, one in 20 get pneumonia, and one in 1000 die. However according to scientists, measles is another potentially eradicable viral infection.The first measles vaccine was introduced in 1963 by John Enders and colleagues - before then almost everyone contracted measles before the age of 15 and the virus killed nearly 500 Americans every year. Subsequently, a very effective combined measles, mumps, and rubella (MMR) vaccine was introduced. By 1999, this virus was considered to be eliminated from the United States. Fifteen years later, however, the Centers for Disease Control and Prevention (CDC) reported that the US has seen its highest number of measles cases (514) since the elimination–and that’s only those reported in the first six months of this year! Measles is mainly considered a childhood disease, but 25 per cent of these reported cases were in 5-19 year olds and 52 per cent were over 20 years of age. Although no measles-related deaths have been reported so far this year, several patients have required hospitalisation due to complications.
Successful vaccination programs need not rely on 100 per cent uptake; ‘herd-’ or ‘community immunity’ occurs when a significant proportion of the population is vaccinated against a disease so that the few who are unvaccinated remain uninfected. This is because chains of infection cannot be maintained through the population. Herd immunity protects people that cannot be vaccinated, for example because of egg allergies (many vaccine strains of viruses are grown in chicken eggs). This immunity can only be maintained if more than 85 per cent of the population is vaccinated, to decrease the likelihood of these chains of infection. Of the measles cases in the US this year, 363 occurred as part of an on-going outbreak in an unvaccinated Amish community in Ohio. The contagiousness of the virus, coupled with the lack of herd immunity, means that infections in this group are very likely. However, isolated communities in the United States are not alone in these measles outbreaks–in 2012 there were more than 2000 cases of measles reported in England and Wales, with the largest epidemic centred in Swansea.
However, herd immunity does not protect the unvaccinated if they leave the herd. Although the MMR vaccine is not immediately brought to mind when considering travel vaccinations, 97 per cent of the recorded infections in the US were linked to foreign travel–particularly to the Philippines. In 2013, 6497 measles cases were reported in the Philippines, 23 of which were fatal. Although some vaccinations are missed due to ignorance or poor health-care, some parents opt to excuse their children from vaccination on the grounds of ‘philosophical exemption’ that is those who do not agree with vaccinations. Those children who have not been vaccinated are relatively safe whilst still in Western countries, but once they embark upon an ever popular gap year, and travel to developing countries, their risk of contracting measles increases dramatically.
The philosophical exemption argument against the MMR vaccination was stirred to life in 1998 by Andrew Wakefield, a physician and researcher. He published an article in The Lancet medical journal linking the administration of the MMR vaccine with the onset of behavioural problems, including autism, in 8 of 12 children. Wakefield actually suggested the use of single vaccines instead of in combination, although much of the press coverage failed to report this accurately. Subsequently, much larger studies have been carried out to try and replicate Wakefield’s findings. One of the largest followed over 537,000 Danish children, 82 per cent of whom had been vaccinated. Although 316 children had a diagnosis of autistic disorder, the authors found no association between vaccination and the development of autism. Following this study, and many others, Wakefield has since been struck from the UK medical register and The Lancet fully retracted the paper in 2010. Even with all this new evidence, there is still a stigma associated with the combination MMR vaccine; a seed of doubt had already been sown.
Contrary to popular opinion, the anti- vaccination movement is not a new one. After Edward Jenner showed that exposure to cow pox could immunise children against infection
by the related but more dangerous small pox virus, vaccination of babies by the age of three months was decreed as law in the UK under the Vaccination Act of 1840. From its introduction, people opposed the law and the Anti-Compulsory Vaccination League was founded in 1867.
A huge anti-vaccination demonstration was held in Leicester in 1885, which attracted 100,000 people and lead to an amendment of the law in 1898. The ‘cumulative penalties’ sub-clause was removed and a ‘conscience’ clause was introduced. This allowed parents who did not believe vaccination was efficacious or safe to obtain a certificate of exemption; this act introduced the concept of the ‘conscientious objector’ into English law.
Perhaps these 19th-century conscientious objectors were justified in their fears; controlled clinical trials had not taken place and the vaccine had not been thoroughly tested. However today’s anti-vaccination campaigners do not have the same arguments to fall back on–vaccines are one of the most thoroughly scrutinised medicines developed nowadays. They undergo four phases of clinical trials over several years, the last of which involves several thousand participants. Some anti-vaccine campaigners argue that the number of vaccines given to children in such a short time is problematic, that they should be spaced out so as not to ‘overwhelm’ the baby’s immune system. However, the antigens presented to a child by vaccinations are a tiny minority compared to the number of bacteria and viruses that a child is exposed to from its parents, a family pet, and the environment. The immune system’s job is to respond to foreign material, and some studies suggest we make over a million specific antibodies in our life time. In the UK, it is advised to immunise your child against eleven different diseases in the first thirteen months, including measles, mumps, and rubella. Vaccines can have some mild side-effects, such as swelling or tenderness at the site of infection, but not having a vaccine is far more frightening, especially if you’re about to embark upon a gap year abroad.
Sarah Smith is a 4th year PhD student at the Wellcome Trust Sanger Institute.