THURSDAY, 1 OCTOBER 2009
 pandemic flu – a global outbreak of the virus – has been a constant presence throughout human history and occurs with a regularity that is chilling. This year it was swine flu, before that we had fears of an avian flu outbreak. This year the effects have been particularly devastating. The World Health Organisation declared swine flu as a global pandemic and there have been over 180,000 cases and 1,400 deaths in more than 100 countries. Even excluding pandemics, each year up to 500,000 people will die from seasonal flu. Although we are unable to halt outbreaks of flu, the latest research may provide us with a weapon to help combat it.
pandemic flu – a global outbreak of the virus – has been a constant presence throughout human history and occurs with a regularity that is chilling. This year it was swine flu, before that we had fears of an avian flu outbreak. This year the effects have been particularly devastating. The World Health Organisation declared swine flu as a global pandemic and there have been over 180,000 cases and 1,400 deaths in more than 100 countries. Even excluding pandemics, each year up to 500,000 people will die from seasonal flu. Although we are unable to halt outbreaks of flu, the latest research may provide us with a weapon to help combat it.Endemic diseases such as bubonic plague, smallpox, cholera and scarlet fever have almost all been eradicated by modern medicine. Science has also helped to prolong the lives of sufferers of deadly diseases such as cancer and AIDS. So why has a cure for flu proved so elusive and why is it so hard to prevent epidemics?
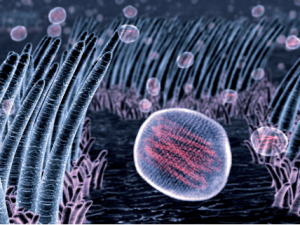
The answer lies in the fact that flu carries its genetic information as RNA. The virus lacks an enzyme to check for errors in its genome, so there is no mechanism to ensure that replication of its RNA remains accurate. The resultant high mutation rate in the RNA allows the virus to continually evolve and hence evade our immune system. In an infected cell, the virus can also exchange genetic material with the host. When this occurs on a large scale, completely new viral strains may emerge to which most people will have little or no resistance, as was the case with swine flu.
Despite these difficulties, science has made some progress in the fight against flu with preventative vaccines – inactive or non-infectious versions of particular strains of the virus. When injected, these cause the immune system to generate antibodies to these weakened strains, priming it to respond quickly to infection by active forms of these same strains and thereby reduce the severity of the symptoms. However, the vaccine only works for the strains present in the shot, which are chosen from among those circulating at the time. The rapid evolution of the virus means that new flu strains constantly emerge, so that the winter flu virus changes composition from year to year and the vaccine administered one year may offer little protection in the next.
Wouldn’t it be better if we could produce a single vaccine that would provide long-term protection against not just current strains, but also new strains of flu? Such is the hope of new research at Warwick University. Nigel Dimmock, professor of virology, has proposed the use of a ‘protecting virus’ to counter flu infections – a synthetic non-infectious virus strain that could protect us from flu for the rest of our lives. The idea sounds a bit like a fantasy; How exactly would willfully infecting yourself with one virus protect you from another?
Dimmock’s new method effectively transforms an active, infectious virus into a vaccination by shortening its genome. A normal influenza virus contains eight separate RNA strands. The protecting virus is identical except for an 80% base deletion on strand one, which renders it harmless: it cannot replicate its RNA or synthesise its protein coating and lacks the genes which code for proteins responsible for infectious symptoms and viral replication.
When a harmful strain of virus is present in the same cell, the genomes of both strains of the virus can be replicated. However, the genome of the protecting virus is shorter than the regular flu virus and its rate of replication consequently higher (the exact ratio remains unclear and may vary from organism to organism). This is the key to preventing infection. The higher replication rate of the protecting virus limits the amount of the harmful virus and the number of cells it infects. Amazingly, the body is protected from all present and future flu strains, because the protecting virus is always replicated faster than any harmful flu virus. It is therefore much more effective than an ordinary vaccination, which only offers protection against specific strains.
Despite its remarkable properties, it is unclear how long such a protecting virus can remain in the body. Experiments carried out by the team at Warwick have shown that the protecting strain is effective even when given up to six weeks before infection. A single dose of current anti-viral drugs like Tamiflu and Relenza gives at most 24 hours of protection. The protecting virus can also work if administered 24 hours after exposure to the active flu virus and may do so following even longer delays. Furthermore, the experiments so far suggest that the infectious virus does not undergo mutation when a protecting virus is present. The reason for this is not entirely clear. However, it does suggest that, even if we were to administer the protecting virus widely, it is unlikely that a superbug would emerge through excessive drug usage.
The protecting virus opens up a new path towards fighting flu and could make it much easier to reduce the chances of future global pandemics occurring. Some flu viruses can cross the species barrier and be carried by birds, pigs or humans. Currently, treating animals, particularly wild ones, is much harder than treating humans. Simply adding the protecting virus to the food and water of animals would massively reduce the cost and effort required to fight infection. Animals that may carry the virus need not be slaughtered and the spread of the virus from country to country could be slowed down or even halted.
Trials still need to be carried out in birds and humans. However, the same concept may help in the fight against similar viral diseases with fast mutation rates, for example, rubella, Dengue fever or even hepatitis B, which are all caused by RNA viruses, if a suitable form of the protecting virus can be made for each one.
C-C Chen is a Part 1b student in the Natural Sciences